A recent Lancet study found 18.1 per cent Covid patients had a psychiatric problem within 14 to 90 days of infection. The Indian Express on how doctors and scientists are trying to unravel the after-effects of SARS-Cov-2 on mental health — from insomnia and anxiety to depression
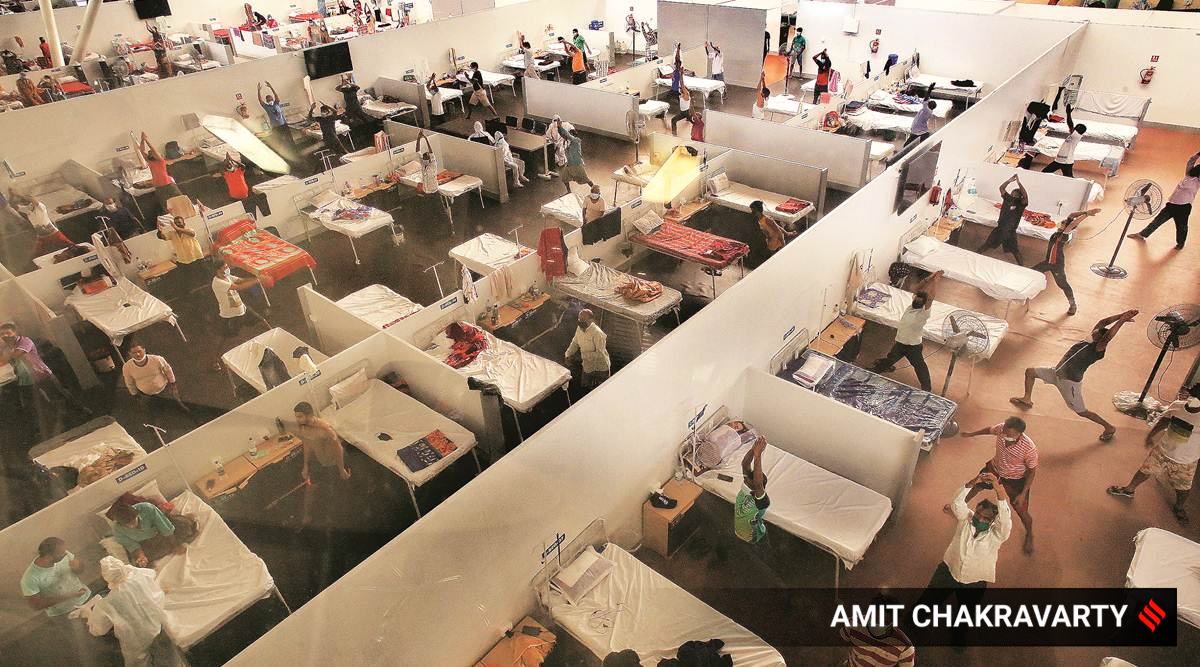 |
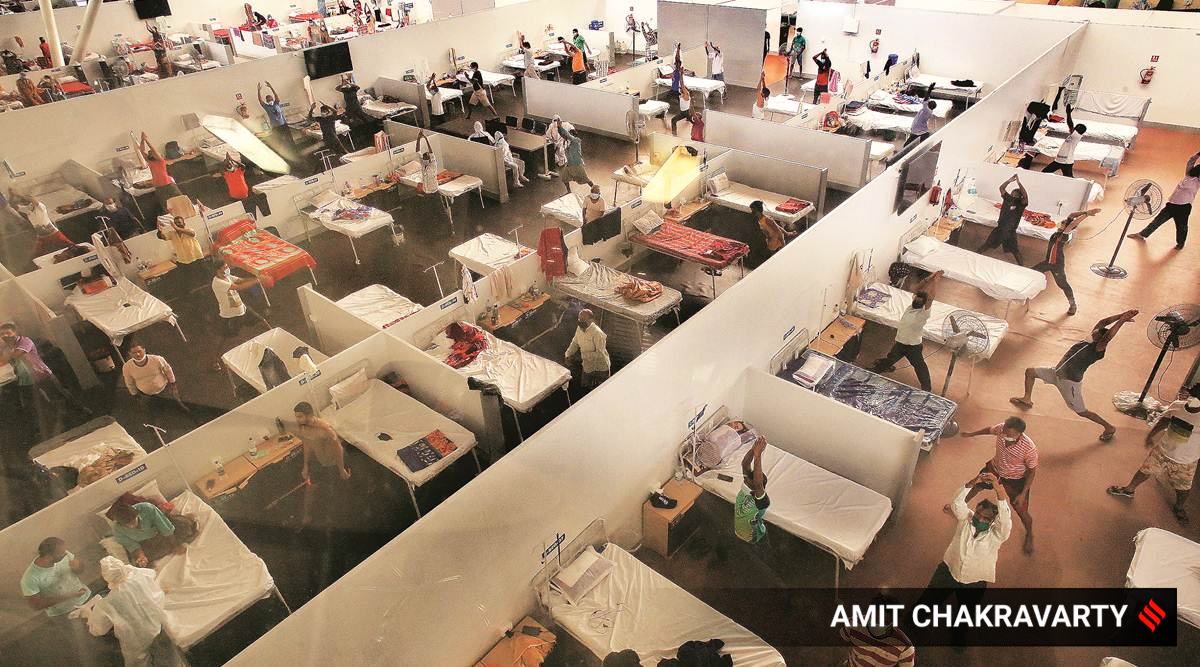
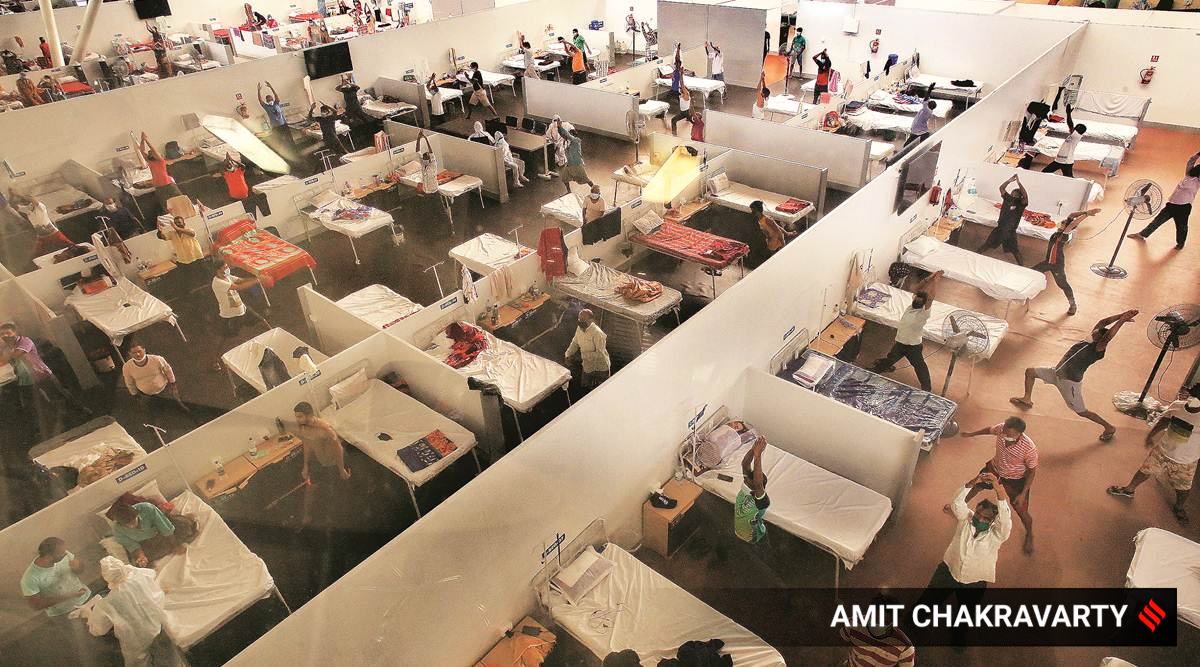
| Residents practise yoga at a Covid care centre in Navi Mumbai. Experts say lack of socialisation and forced isolation have increased sense of loneliness. |
Tabassum Barnagarwala | IE | November 15, 2020 : Dr Jalil Parkar has treated more than 1,400 Covid-19 patients since March 11. By early June, by which time he had seen some 200 critical Covid cases being rushed in to Mumbai’s Lilavati Hospital, where he is a senior pulmonologist, he thought he knew “the a-b-c-d of the virus”. So if he ever felt the symptoms himself, he thought, his plan of action would kick in effortlessly, one that he had prescribed to each of his patients — the usual ivermectin (antiparasitic drug) and doxycycline (antibiotic).But when he was diagnosed with Covid-19, the 62-year-old realised he had underestimated the virus. A diabetic, Parkar says the virus not only “ravaged” his lungs but also attacked his central nervous system. Parkar is considered a celebrity doctor in Mumbai, with the late Balasaheb Thackeray, actor Dilip Kumar and Sanjay Dutt, among others, as his patients. As he announced Thackeray’s death to an emotionally charged media in November 2013, many had noted how calm and composed he was. “I rarely cry, except when my mother died. But Covid-19 was pure trauma… like seeing death and coming out of it. While I was hospital with Covid, I would break down and cry every time a colleague called me,” he says. After discharge, while under quarantine, Parkar says he would often lose track of what he was doing. Just the inability to smell or taste his coffee every morning irritated him. And besides, there was an inexplicable “fear” that lurked somewhere in his mind.
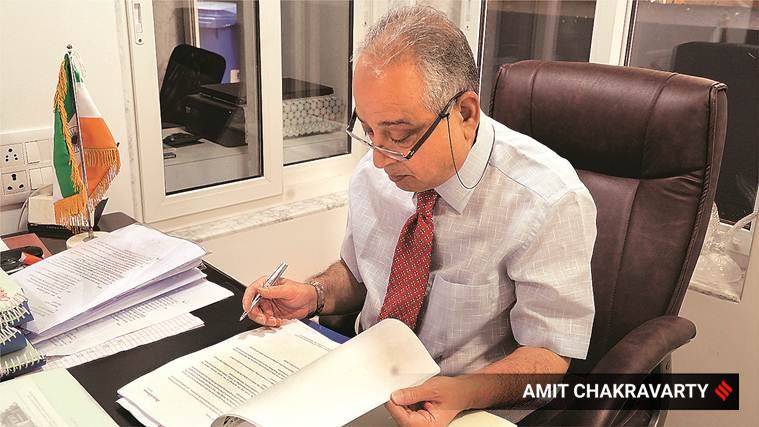 Dr Jalil Parkar says post-Covid, he had instances of confusion and memory loss
Dr Jalil Parkar says post-Covid, he had instances of confusion and memory loss
Of all the unknowns that accompany SARS-Cov-2 — the virus that’s known to cause Covid-19, one that’s 1,200 times smaller than the diameter of a hair strand and an invisible speck to the human eye — the least discussed is what it does to the human mind. Long Covid, now a common phrase for prolonged post-Covid complications for those who have recovered from the infection, is now becoming a larger burden than actively infected cases. In India, there are 4.89 lakh active Covid cases and 8 million of those who have recovered. While there is no systematic process to track each one of them, given the numbers, doctors say several patients have been returning with complaints of prolonged fatigue, headaches, insomnia, shortness of breath, body pain, muscle pain, lack of appetite, sore throat and even diarrhoea. Add to that, mental health issues.There is now increasing evidence that Covid-19, apart from causing lung, heart and kidney damage, can lead to anxiety, depression, psychosis, insomnia and memory fogs, making a person forgetful and disoriented.A Lancet Psychiatry study published last week found that 18.1 per cent Covid patients had a psychiatric problem within 14 to 90 days of infection;In Parkar’s case, he says that while there were instances of confusion and memory loss, they were not serious enough and he eventually did remember details. EXPLAINED While Long Covid is a global phenomenon, the evidence of post-Covid mental illness is particularly alarming for India given how it is already sitting on a mental health landmine. Consider this : The National Mental Health Survey (NMHS), 2016, indicates that 14 per cent of India's population require active mental health intervention n While India needs one psychiatrist per lakh population, as the NMHS survey shows, most states, except Kerala, fall short of this requirement. Madhya Pradesh is the worst with 0.05 psychiatrist per lakh population; Kerala has 1.12. “The limited availability of specialist mental health human resources (psychiatrists, clinical psychologists and psychiatric social workers)... has been one of the barriers in providing essential mental health care to all,” the NMHS report observes. Maharashtra’s Public Health Department that handles primary health centres, rural and district hospitals across the state, has only 44 psychiatrists to run the District Mental Health Programme. Data till November 9 shows 19,287 Covid-19 patients and health workers have been provided psychological counselling to deal with the pandemic. In Sir JJ Group of Hospitals, the largest state-run hospital in Maharashtra, there are only six psychiatrists to attend to the 200-odd patients who visit its OPD daily. Here, a psychiatrist visits a Covid-19 ward twice a week to do group counselling and individual counselling. “The group counselling is for 15-20 minutes. We train patients to do coping and relaxation exercise. But if we had more psychiatrists, individual attention could be improved,” a psychiatrist from the hospital said. Once a patient is discharged, there is no follow-up. Eight months into the pandemic, only a few hospitals have a full-fledged post-Covid OPD clinic. It is not unusual for viruses to cause neurological changes in the brain. There’s evidence that some patients of both Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), predecessors of Covid-19, had anxiety, insomnia, memory loss and manic symptoms.A hundred years ago, the Spanish flu that killed over 50 million globally, also affected parts of the brain, especially the pons, basal ganglia, midbrain and cranial nerve. Autopsies of patients have shown brain damage and recovered patients have been documented with obstructive compulsive disorder (OCD) for years. Several others have exhibited a disorder similar to Parkinson’s disease.; Professor Paul J Harrison from the Department of Psychiatry, University of Oxford, co-author of a large cohort study covering 62,354 Covid patients that was published in The Lancet Psychiatry last week, told The Sunday Express that while they noticed a definite correlation between Covid and mental health, there are several questions that remain unanswered. Like whether these neurological changes are different for different age groups and for rural/urban population, or whether it could result in Parkinson’s-like disorders.Dr Rajesh Parikh, neuro-psychiatrist and Director of Medical Research at Mumbai’s Jaslok Hospital and co-author of the recently released The Corona Virus — What You Need to Know About the Global Pandemic, says, “We are seeing three categories of patients: first, where the coronavirus directly affects the brain; second of people with existing mental health problems; and the third, where mental health issues are caused by the viral infection’s complications.” In the first case, Parikh says, the coronavirus gains direct and quick entry through the olfactory nerve (responsible for sense of smell) into the brain. Once the virus enters the brain, the spike proteins on the virus’s surface lock with ACE-2 receptors and enter brain cells. “Because the virus can get direct access to the brain through the olfactory nerve, many Covid-19 patients have loss of smell. But in some cases, mental disturbance could be the first signs of Covid-19 infection, even before loss of smell, taste or fever,” Parikh says.Now that the virus has begun its onslaught, the body’s immune system stirs awake and releases cytokines to fight back. But cytokines, Parikh explains, are also known to cause inflammation and affect neurotransmitters like serotonin, dopamine and glutamate in the brain. Serotonin and dopamine are happy or feel-good hormones, and glutamate is key to learning and memory. A disruption in their levels due to cytokines can cause depression, delirium and memory loss. A patient may not realise the time of day, who they are talking to, what they were doing.Parikh says patients with existing mental health illness already have lower immunity and are thus more vulnerable to the virus. Once infected, their mental illness is aggravated by the virus.Patients may also struggle with survivor’s guilt (after losing a family member to Covid) or display anxiety over whether they will survive the infection. “This is what we call post-traumatic stress disorder (PTSD) and post-intensive care syndrome (PICS),” says Parikh. This is what the Gawdes went through. In October, Madhukar and Madhumati Gawde contracted Covid-19. While 60-year-old Madhumati, who is diabetic, had to be admitted to Mumbai’s Apex Hospital, Madhukar was taken to a civic isolation centre in Mulund, in Mumbai’s eastern suburb. They never saw each other again. Madhumati, who stayed critical and on ventilator support for long, passed away a fortnight ago. “Since then, he (Madhukar) hasn’t been sleeping. He doesn’t pay attention when we are talking and does not talk much himself. It’s as if his mind is elsewhere. He keeps saying if he were not in isolation, he would have saved his wife. He is now on anti-anxiety medication,” says Madhukar’s son-in-law Amit Aparaj.In his book, Parikh has written about one of his patients — a 35-year-old fitness trainer who required critical care due to Covid-19 for an entire month. At the end of it, the trainer had muscle weakness and difficulty moving. For someone whose life revolved around staying fit, his weak muscles now became a cause for depression, fear and nightmares.The BYL Nair Hospital in Mumbai has seen three cases of psychosis in women who had Covid-19 and who had given birth in the hospital. The women suffered postpartum depression, as several mothers do after child birth, but in this case they also became ‘delusional’. The hospital treated the three with anti-psychiatric drugs and they recovered in about a week.
Every Covid-19 patient Dr Rahul Pandit treats in Fortis Hospital, he makes it a point to counsel them about possible signs of worsening mental health. An intensivist and a member of the Maharashtra state task force for Covid, Pandit has personal experience to vouch for. While he contracted Covid-19 in May, he did not realise he was battling a severe post-Covid mental disorder until he came out of it.
“I just couldn’t sleep, I thought about Covid all the time, there was constant fatigue. Only after it settled down did I realise these were neuro-psychiatric symptoms,” says Pandit, 47.
Pandit, who has treated several politicians for Covid-19, including former Maharashtra CM Devendra Fadnavis and current state housing minister Jitendra Awhad, is a case in point to show how hard it can be to detect psychiatric disturbances even for medical practitioners.
Pandit says psychiatric episodes are more common in Covid-19 patients admitted to ICUs than those isolated at home.
Even after two months of getting infected, former Jalna MLA Arjun Khotkar, Shiv Sena leader and a former minister, continues to feel the after-effects. “It’s is very difficult to put in words what I am feeling…,” he says. “Chidchida rehta hun har samay (I am frustrated all the time).”
“By afternoon, I forget what I ate in the morning. I was used to working for 12 hours straight. Now by 2.30 pm, I want people to leave me alone. i got panicky if people surround me. I just want to sleep" , he says.
Doctors and experts say the unpredictability of the virus — with symptoms ranging from none to mild flu-like irritation to more debilitating illnesses and finally, at the other end of the spectrum, death — is what is adding a mental dimension to the disease. Add to that the isolation that patients go through in disease and death, and the fact that measures by governments to check the spread of the virus have had economic ramifications in the form of job losses and salary cuts.
Dr Shubhangi Parkar, former head of KEM Psychiatry Department, says she has been seeing several cases of Covid patients having to deal with the stress of job loss or insecurity at work. “The pandemic has led to financial losses. Those already in financial distress find the stress hard to deal with if they also get infected with Covid,” she says, adding that a combination of external factors are at play. “Lack of socialisation and forced isolation have increased the sense of loneliness.”
For now, doctors say they don’t know how long it will take for Covid patients to recover fully, except that most of them will need some kind of support. “We are only beginning to understand the impact of post-acute Covid, including psychiatry. What we know is that it lasts, but for how long, we don’t know yet,” says Parikh, the neuro-psychiatrist at Jaslok.

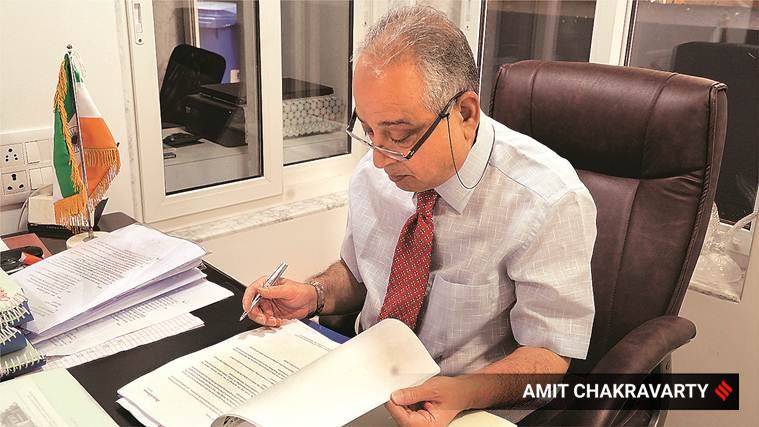 Dr Jalil Parkar says post-Covid, he had instances of confusion and memory loss
Dr Jalil Parkar says post-Covid, he had instances of confusion and memory loss

0 Response to "Covid’s X factor- after-effects of SARS-Cov-2 on mental health — from insomnia and anxiety to depression"
Post a Comment
Disclaimer Note:
The views expressed in the articles published here are solely those of the author and do not necessarily reflect the official policy, position, or perspective of Kalimpong News or KalimNews. Kalimpong News and KalimNews disclaim all liability for the published or posted articles, news, and information and assume no responsibility for the accuracy or validity of the content.
Kalimpong News is a non-profit online news platform managed by KalimNews and operated under the Kalimpong Press Club.
Comment Policy:
We encourage respectful and constructive discussions. Please ensure decency while commenting and register with your email ID to participate.
Note: only a member of this blog may post a comment.